Understanding Piriformis Syndrome
Piriformis syndrome involves the piriformis muscle compressing the sciatic nerve‚ leading to pain and potential numbness; understanding its causes is crucial for effective management․
The piriformis muscle‚ located deep in the buttock‚ can irritate the sciatic nerve‚ causing pain radiating down the leg‚ impacting daily activities and requiring targeted exercises․
Various factors‚ including muscle tightness‚ overuse‚ or anatomical variations‚ contribute to piriformis syndrome; identifying these risks helps in preventing and treating the condition effectively․
What is Piriformis Syndrome?
Piriformis syndrome is a relatively uncommon condition characterized by irritation of the sciatic nerve due to compression from the piriformis muscle․ This muscle‚ situated deep within the buttock‚ plays a role in hip rotation and stabilization․ When the piriformis muscle becomes tight or spasms‚ it can impinge upon the sciatic nerve‚ which runs nearby․
This compression leads to a variety of symptoms‚ most notably pain in the buttock region that may radiate down the leg‚ mimicking sciatica․ However‚ unlike typical sciatica caused by spinal issues‚ piriformis syndrome originates from a muscular source․ The condition isn’t always easily diagnosed‚ often requiring careful evaluation to rule out other potential causes of sciatic-like pain․
Effective management often involves a combination of stretching‚ strengthening‚ and nerve gliding exercises‚ with resources available through the NHS and reputable physiotherapy websites․
Anatomy of the Piriformis Muscle
The piriformis muscle is a flat‚ band-like muscle located in the gluteal region‚ deep to the gluteus maximus․ Originating from the sacrum‚ it passes through the greater sciatic foramen and attaches to the greater trochanter of the femur․ Its primary functions include external rotation of the hip joint and abduction when the hip is flexed․
Crucially‚ the sciatic nerve passes either beneath‚ through‚ or even within the piriformis muscle in approximately one-third of the population‚ making it vulnerable to compression․ Variations in this anatomical relationship explain why some individuals are more prone to piriformis syndrome․ Understanding this anatomy is vital when considering exercises․
Proper stretching and strengthening of the piriformis‚ alongside surrounding muscles‚ can help alleviate nerve compression and restore optimal hip function‚ as detailed in NHS resources․
Causes and Risk Factors
Piriformis syndrome arises from compression or irritation of the sciatic nerve by the piriformis muscle․ Common causes include muscle spasms‚ tightness due to overuse‚ or anatomical variations where the sciatic nerve passes directly through the muscle․ Prolonged sitting‚ especially with poor posture‚ significantly contributes to muscle imbalances․
Risk factors encompass activities involving repetitive hip movements‚ like running or cycling‚ and conditions causing inflammation in the area․ Direct trauma to the buttock can also trigger the syndrome․ Individuals with pre-existing spinal issues may be more susceptible․
The NHS emphasizes identifying these factors to tailor exercise programs‚ focusing on stretching and strengthening to restore proper biomechanics and alleviate nerve compression․

Symptoms of Piriformis Syndrome
Piriformis syndrome typically presents as deep buttock pain‚ potentially radiating down the leg‚ mimicking sciatica; numbness and tingling are also common symptoms․
Pain often worsens with prolonged sitting‚ climbing stairs‚ or running‚ impacting daily activities; the NHS provides resources for symptom recognition and management․
Symptoms vary in intensity‚ ranging from mild discomfort to debilitating pain‚ requiring tailored exercise plans to address individual needs and improve function․
Pain Location and Characteristics
Piriformis syndrome pain is commonly felt deep within the buttock‚ often on one side‚ though it can be bilateral in some cases․ This discomfort frequently radiates downwards‚ potentially mimicking sciatica‚ extending along the path of the sciatic nerve – down the back of the thigh‚ and even into the calf and foot․
The pain’s characteristics can vary significantly․ Some individuals describe it as a dull ache‚ while others experience sharp‚ stabbing sensations․ Prolonged sitting‚ especially on hard surfaces‚ often exacerbates the pain‚ as does climbing stairs or engaging in activities that involve hip rotation․ The NHS emphasizes recognizing these patterns․
Pain may be triggered by direct pressure on the piriformis muscle․ It’s often worsened by activities that compress the nerve‚ and can be accompanied by a feeling of tightness or spasm in the buttock region․ Understanding these pain characteristics is vital for accurate diagnosis and targeted exercise selection‚ as outlined in NHS resources and physiotherapy guides․
Numbness and Tingling
Piriformis syndrome frequently presents with numbness and tingling sensations‚ often following the distribution of the sciatic nerve․ This means individuals may experience these symptoms in the back of the thigh‚ calf‚ foot‚ and even toes․ The intensity can range from mild prickling to a more pronounced loss of sensation․
These neurological symptoms arise from the compression or irritation of the sciatic nerve by the piriformis muscle․ Prolonged compression can disrupt nerve signals‚ leading to altered sensation․ The NHS highlights that these symptoms aren’t always constant and can fluctuate with activity levels․
NHS guidance and physiotherapy resources emphasize differentiating these sensations from those caused by other conditions․ While exercises can help alleviate pressure‚ persistent or worsening numbness warrants medical evaluation․ Recognizing the pattern and location of these symptoms is crucial for effective management and targeted exercise programs․
Impact on Daily Activities
Piriformis syndrome can significantly disrupt daily life‚ impacting a wide range of activities․ Simple actions like walking‚ running‚ or even sitting for extended periods can exacerbate pain and discomfort․ The NHS acknowledges that this can lead to limitations in work‚ exercise‚ and social engagements․
Individuals may find it difficult to climb stairs‚ get in and out of cars‚ or participate in activities requiring hip rotation․ Prolonged sitting often worsens symptoms due to continued pressure on the sciatic nerve․ The NHS emphasizes the importance of activity modification and targeted exercises․
NHS resources and physiotherapy guides often recommend strategies to minimize these impacts‚ including ergonomic adjustments and a gradual return to activity․ Understanding these limitations is crucial for developing a personalized management plan and improving quality of life․

Diagnosis of Piriformis Syndrome
Diagnosis involves a physical exam‚ ruling out sciatica or spinal stenosis; NHS guidance emphasizes careful assessment before recommending specific exercise programs․
NHS doctors may use imaging like MRI‚ though it’s not always conclusive; accurate diagnosis is key for effective exercise-based rehabilitation․
EMG testing can help confirm nerve involvement; the NHS prioritizes a thorough evaluation to tailor exercise plans to individual needs․
Physical Examination
A comprehensive physical examination is the cornerstone of diagnosing piriformis syndrome‚ as highlighted by NHS protocols․ This involves assessing a patient’s range of motion in the hip‚ evaluating muscle strength‚ and palpating the piriformis muscle for tenderness․ Specific provocative tests‚ like the FAIR test (Flexion‚ Adduction‚ Internal Rotation)‚ are employed to reproduce the patient’s pain and identify piriformis involvement․
The NHS emphasizes a detailed neurological assessment to rule out nerve root compression from other sources․ This includes testing reflexes‚ sensation‚ and muscle strength in the lower limb․ Healthcare professionals will also inquire about the patient’s medical history and activity levels to understand potential contributing factors․ The findings from the physical exam guide the development of an individualized exercise plan‚ often incorporating stretches and strengthening exercises‚ potentially sourced from NHS-approved resources or reputable physiotherapy websites․
Ruling Out Other Conditions (Sciatica‚ Spinal Stenosis)
Differentiating piriformis syndrome from sciatica and spinal stenosis is crucial for accurate diagnosis‚ aligning with NHS best practices․ Sciatica‚ often caused by a herniated disc‚ presents similar leg pain but originates from nerve compression in the spine․ Spinal stenosis involves narrowing of the spinal canal‚ also causing leg symptoms․
The NHS utilizes a thorough assessment to distinguish these conditions․ This includes evaluating the pain’s specific location‚ quality‚ and aggravating factors․ Neurological examinations‚ assessing reflexes and sensation‚ help pinpoint the source of nerve compression․ Imaging‚ like MRI‚ may be necessary to visualize the spine and rule out structural issues․ Accurate diagnosis ensures appropriate treatment‚ avoiding ineffective exercises for conditions other than piriformis syndrome‚ and guiding patients towards relevant NHS resources․
Imaging Techniques (MRI‚ EMG ー when necessary)
While often diagnosed clinically‚ imaging techniques like MRI can aid in confirming piriformis syndrome and excluding other pathologies‚ aligning with NHS diagnostic protocols․ MRI visualizes soft tissues‚ helping identify piriformis muscle abnormalities or sciatic nerve compression․ However‚ MRI findings aren’t always conclusive‚ as the syndrome often lacks distinct structural changes․
Electromyography (EMG) is reserved for complex cases where nerve function assessment is needed․ EMG measures electrical activity in muscles‚ detecting nerve damage or dysfunction․ The NHS typically employs these tests judiciously‚ prioritizing clinical evaluation and conservative management initially․ Accessing reliable PDF resources from NHS physiotherapy departments can clarify when and why these imaging techniques are utilized‚ ensuring informed patient understanding․

NHS Approach to Piriformis Syndrome
The NHS prioritizes initial assessment‚ conservative management—including tailored exercise programs—and referral to physiotherapy‚ often providing accessible PDF exercise guides․
NHS pathways involve consultation‚ physical examination‚ and potentially imaging; exercise is central‚ with resources available online and through physiotherapy services․
Treatment focuses on pain relief‚ restoring function‚ and preventing recurrence‚ utilizing evidence-based exercises detailed in NHS-approved PDF materials․
Initial Consultation and Assessment
The first step within the NHS involves a comprehensive consultation with a healthcare professional‚ typically a GP or physiotherapist․ This initial assessment focuses on gathering a detailed medical history‚ exploring the onset‚ location‚ and characteristics of your pain‚ and understanding how it impacts your daily activities;
A thorough physical examination is then conducted‚ evaluating your range of motion‚ muscle strength‚ and nerve function․ Specific tests are performed to assess the piriformis muscle and sciatic nerve‚ helping to differentiate piriformis syndrome from other conditions like sciatica or spinal stenosis․
The NHS may provide preliminary advice on self-management strategies‚ including gentle stretches and activity modification‚ and potentially direct you to relevant PDF resources detailing appropriate exercises․ This initial assessment informs the development of a personalized treatment plan‚ often incorporating a structured exercise program․
Referral Pathways
If your GP suspects piriformis syndrome‚ referral to a physiotherapist is a common pathway within the NHS․ Physiotherapists are specialists in musculoskeletal conditions and can provide a detailed assessment and tailored exercise program‚ often including PDF guides for home practice․
In some cases‚ particularly if the diagnosis is unclear or other conditions need to be ruled out‚ referral to a specialist‚ such as a neurologist or orthopaedic surgeon‚ may be necessary․ This ensures a comprehensive evaluation and accurate diagnosis․
The NHS also offers access to pain management clinics for individuals experiencing persistent or severe pain․ These clinics may employ a multidisciplinary approach‚ combining exercise therapy with other interventions․ Accessing NHS resources often begins with a GP referral‚ streamlining the process․
Conservative Management Strategies
The initial approach within the NHS for piriformis syndrome focuses on conservative management․ This typically involves a combination of physiotherapy‚ exercise‚ and pain relief strategies‚ often utilizing downloadable PDF exercise guides․
Physiotherapy aims to restore normal muscle function and reduce nerve compression through targeted stretching and strengthening exercises․ Pain management may include over-the-counter analgesics or‚ in some cases‚ short-term use of muscle relaxants prescribed by a GP․
Activity modification is also key‚ avoiding activities that aggravate symptoms․ The NHS emphasizes self-management strategies‚ empowering patients with exercises and advice for long-term symptom control and prevention of recurrence․

Piriformis Syndrome Exercises: A Core Component of Treatment
Targeted exercises‚ often available as NHS PDFs‚ are vital for relieving compression and pain․ Stretching and strengthening routines help restore muscle balance and nerve function․
Stretching Exercises
Stretching plays a pivotal role in alleviating piriformis syndrome symptoms‚ gently lengthening the muscle and reducing sciatic nerve compression․ The NHS often provides PDF guides detailing effective stretches․
The Piriformis Stretch (Figure Four Stretch) involves lying on your back‚ crossing one ankle over the opposite knee‚ and gently pulling the uncrossed thigh towards your chest․ Knee-to-Chest Stretches are also beneficial‚ drawing both knees towards the chest while lying supine․
A Seated Piriformis Stretch can be performed by sitting with legs extended‚ bending one knee‚ and rotating it towards the opposite side‚ leaning forward slightly․ These stretches‚ when performed correctly and consistently‚ can significantly improve flexibility and reduce discomfort‚ as outlined in many NHS resources․
Piriformis Stretch (Figure Four Stretch)
The Piriformis Stretch‚ often called the Figure Four Stretch‚ is a cornerstone of NHS-recommended exercises for piriformis syndrome‚ frequently detailed in their PDF guides․ Begin by lying on your back with knees bent and feet flat․
Cross your affected side ankle over the opposite knee‚ forming a “figure four” shape․ Gently pull the thigh of the uncrossed leg towards your chest‚ holding the stretch for 20-30 seconds․ You should feel a stretch deep in the buttock of the crossed leg․
Repeat this 2-3 times‚ ensuring a comfortable stretch without causing pain․ Proper form‚ as illustrated in NHS resources‚ is crucial for maximizing effectiveness and preventing injury․
Knee-to-Chest Stretch
The Knee-to-Chest Stretch is a foundational exercise often included in NHS physiotherapy PDFs for managing piriformis syndrome․ Begin by lying on your back with your knees bent and feet flat on the floor․
Gently pull one knee towards your chest‚ keeping the other foot flat or extended․ Hold this position for 20-30 seconds‚ feeling a gentle stretch in your lower back and potentially the buttock area․
Repeat with the other leg‚ alternating several times․ This stretch helps to relieve tension in the lower back and hips‚ indirectly addressing piriformis muscle tightness․ NHS guidance emphasizes controlled movements and avoiding any sharp pain․
Seated Piriformis Stretch
The Seated Piriformis Stretch‚ frequently detailed in NHS-approved PDF exercise guides‚ offers a convenient way to alleviate tension․ Sit upright on a chair with your feet flat․
Cross the affected leg over the opposite knee‚ forming a figure-four shape․ Gently lean forward from your hips‚ keeping your back straight‚ until you feel a stretch in your buttock․
Hold this position for 20-30 seconds‚ breathing deeply․ Repeat several times on each side․ The NHS recommends maintaining a comfortable stretch‚ avoiding any forceful movements or pain․ This stretch targets the piriformis muscle directly‚ promoting flexibility and reducing nerve compression․
Strengthening Exercises
NHS PDF resources emphasize strengthening exercises as vital for long-term piriformis syndrome management․ Weak glutes contribute to the problem‚ so building strength is key․
Glute Bridges effectively target the gluteal muscles; lie on your back with knees bent and lift your hips off the floor‚ squeezing your glutes at the top․
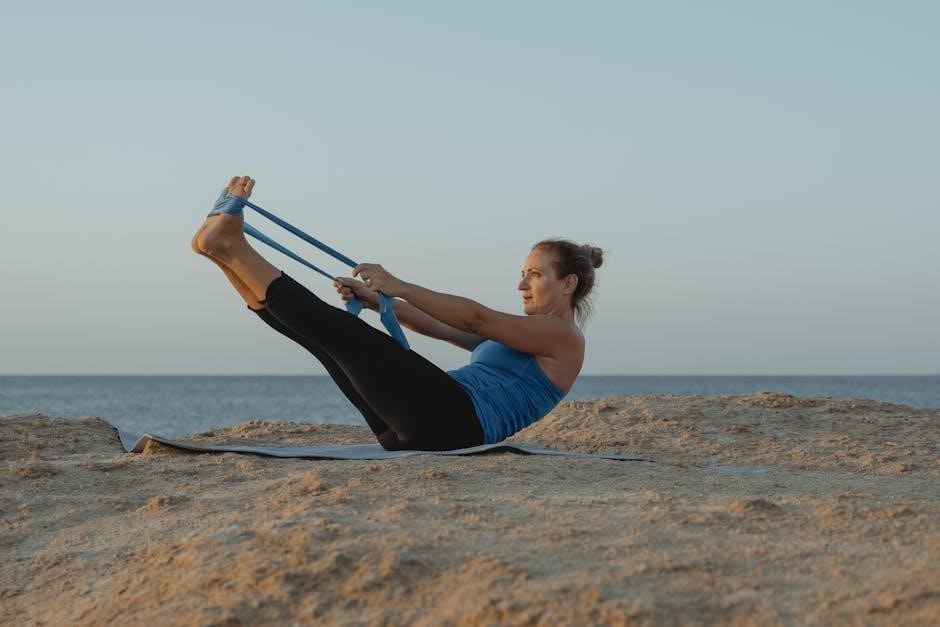
Clamshells‚ using a resistance band around your knees‚ strengthen hip abductors․ Hip Abduction Exercises‚ like side leg raises‚ further enhance stability․ These exercises improve hip control‚ reducing stress on the piriformis muscle and sciatic nerve․
Glute Bridges
NHS PDF guides frequently recommend Glute Bridges as a foundational strengthening exercise for piriformis syndrome․ This exercise directly targets the gluteus maximus‚ a key muscle for hip extension and stabilization․
To perform‚ lie on your back with knees bent and feet flat on the floor․ Engage your core and glutes‚ then lift your hips off the ground‚ forming a straight line from shoulders to knees․
Hold briefly at the top‚ squeezing your glutes‚ then slowly lower back down․ Repeat 10-15 times for 2-3 sets․ Proper form is crucial; avoid arching your back excessively․
Clamshells
Clamshells are a commonly prescribed exercise within NHS-recommended PDF rehabilitation programs for piriformis syndrome‚ focusing on strengthening hip external rotators․ This targets the gluteus medius‚ crucial for pelvic stability․
Lie on your side with knees bent and stacked‚ feet together․ Keeping your feet touching‚ lift your top knee away from the bottom knee‚ like opening a clamshell․

Maintain a neutral spine and avoid rotating your pelvis․ Hold briefly‚ then slowly lower your knee back down․ Perform 10-15 repetitions on each side for 2-3 sets․ Resistance bands can increase the challenge․
Hip Abduction Exercises
Hip abduction exercises‚ frequently detailed in NHS PDF guides for piriformis syndrome‚ aim to strengthen the gluteus medius and minimus – key muscles for hip stability and preventing further irritation of the sciatic nerve․
These exercises involve moving your leg away from the midline of your body․ Side-lying leg raises are a common variation; lie on your side and lift your top leg‚ keeping it straight and controlled․
Alternatively‚ use resistance bands around your ankles for added challenge․ Perform 10-15 repetitions on each leg for 2-3 sets‚ focusing on slow‚ controlled movements․ Proper form is essential․
Nerve Flossing Exercises
Nerve flossing exercises‚ often included in NHS-recommended PDF resources for piriformis syndrome‚ gently mobilize the sciatic nerve‚ reducing compression and alleviating associated pain and numbness․ These techniques aren’t stretches‚ but movements․
A common technique involves seated positions‚ alternating between flexing and extending the foot while tilting the head to opposite sides․ This creates tension and release along the nerve pathway․
The goal is gentle mobilization‚ not forceful stretching․ Perform these exercises slowly and cautiously‚ stopping if you experience increased pain․ Repetitions should be controlled‚ typically 10-15 per session‚ several times daily․
Sciatic Nerve Floss (Gentle Mobilization)
Sciatic nerve floss‚ detailed in many NHS-approved PDF guides for piriformis syndrome‚ is a technique to gently move the sciatic nerve through its pathway․ Begin seated with legs extended․ Flex your foot‚ point your toes towards your shin‚ and simultaneously tilt your chin towards your chest․
Then‚ extend your knee‚ point your toes‚ and look up․ Repeat this sequence rhythmically‚ creating a “flossing” motion along the nerve․ Focus on gentle movements; avoid sharp pain․
The NHS emphasizes controlled repetitions (10-15) several times daily․ Proper form is crucial; consult a physiotherapist if unsure․ This exercise aims to reduce nerve irritation‚ not to stretch the nerve itself․
Benefits of Nerve Flossing
Nerve flossing‚ often included in NHS-recommended PDF resources for piriformis syndrome‚ offers several benefits․ It gently mobilizes the sciatic nerve‚ reducing adhesion and improving its gliding motion within surrounding tissues․ This can alleviate pain‚ numbness‚ and tingling associated with nerve compression․
By restoring optimal nerve movement‚ flossing can improve nerve conductivity and function․ The NHS highlights that consistent‚ gentle flossing can decrease inflammation around the nerve․
It’s crucial to perform the exercise correctly‚ avoiding overstretching․ Combining nerve flossing with other exercises‚ like stretching and strengthening‚ maximizes its effectiveness in managing piriformis syndrome symptoms․

Finding Piriformis Syndrome Exercises PDF Resources (NHS & Reliable Sources)
NHS websites and reputable physiotherapy sources offer downloadable PDF guides detailing piriformis syndrome exercises‚ ensuring safe and effective rehabilitation programs․
Accessing these resources provides structured exercise plans‚ promoting consistent practice and optimal recovery from piriformis-related discomfort and limitations․
Always prioritize guides from trusted healthcare providers to guarantee accuracy and suitability for your specific condition and needs․
NHS Website Resources
The National Health Service (NHS) provides a wealth of information regarding piriformis syndrome‚ though dedicated PDF exercise guides are not always directly available for download․ However‚ the NHS website offers comprehensive details on the condition‚ its symptoms‚ and general advice for self-management․
Patients can find information on appropriate stretching and strengthening exercises‚ often illustrated with clear diagrams‚ that can be adapted into a personal rehabilitation plan․ The NHS emphasizes conservative management strategies‚ including physiotherapy‚ as the first line of treatment․
While a single downloadable PDF may not exist‚ the website directs individuals to relevant physiotherapy exercises and provides links to trusted organizations offering further resources․ It’s crucial to consult with a healthcare professional for a personalized exercise program tailored to your specific needs and severity of symptoms‚ ensuring safe and effective recovery․
Reputable Physiotherapy Websites
Several reputable physiotherapy websites offer downloadable PDF exercise guides specifically for piriformis syndrome․ These resources often provide detailed instructions and illustrations for stretching and strengthening exercises targeting the piriformis muscle and surrounding structures․
Websites like PhysioWorks and similar platforms created by qualified physiotherapists frequently feature comprehensive rehabilitation programs․ These guides typically include exercises like the figure-four stretch‚ knee-to-chest stretches‚ glute bridges‚ and clamshells‚ all designed to alleviate pain and restore function․
Always ensure the website is run by licensed professionals and provides evidence-based information․ Prioritize resources that emphasize proper form and progression‚ and consult with your own physiotherapist before starting any new exercise program to ensure it’s appropriate for your individual condition․
Evaluating the Quality of Online Exercise Guides
When sourcing PDF exercise guides for piriformis syndrome‚ particularly from online sources‚ critical evaluation is essential․ Prioritize guides created by qualified healthcare professionals – physiotherapists or medical doctors – ensuring expertise and accuracy․
Look for guides that clearly explain the rationale behind each exercise‚ detailing the muscles targeted and the expected benefits․ High-quality resources will emphasize proper form‚ offering visual aids like images or videos‚ and providing modifications for different fitness levels․
Beware of guides lacking author credentials or promoting overly aggressive exercises․ Cross-reference information with reputable sources like the NHS website and consult your healthcare provider before implementing any new exercise regimen․

Long-Term Management and Prevention
Consistent exercise‚ maintaining flexibility‚ and ergonomic adjustments are vital for long-term relief; NHS resources offer PDF guides for sustained muscle health and prevention․
Regular stretching and strengthening‚ alongside mindful activity modification‚ help prevent recurrence; prioritize proper posture and listen to your body’s signals for lasting comfort․
Proactive management‚ incorporating NHS-recommended exercises‚ minimizes irritation and supports ongoing well-being‚ reducing the risk of future piriformis syndrome episodes․
Maintaining Flexibility and Strength
Consistent engagement with targeted exercises is paramount for long-term management of piriformis syndrome‚ preventing recurrence and improving overall function․ The NHS provides valuable PDF resources detailing stretching routines‚ like the figure-four stretch and knee-to-chest exercises‚ designed to alleviate muscle tension around the piriformis and sciatic nerve․
Alongside stretching‚ strengthening exercises‚ such as glute bridges and clamshells‚ are crucial for supporting the hip and stabilizing the pelvis․ These exercises enhance muscle balance‚ reducing strain on the piriformis․ Regularly performing these routines‚ guided by NHS recommendations‚ builds resilience and minimizes the likelihood of future irritation․ Prioritizing both flexibility and strength ensures a holistic approach to managing this condition‚ promoting sustained comfort and mobility․
Ergonomic Considerations
Addressing postural habits and workspace setup is vital in managing piriformis syndrome‚ complementing exercise routines detailed in NHS PDF guides․ Prolonged sitting‚ particularly with poor posture‚ can exacerbate muscle imbalances and nerve compression․ Optimizing your workstation with an ergonomic chair offering lumbar support is essential․
Ensure your hips and knees are at a 90-degree angle‚ and feet are flat on the floor․ Regular breaks to stand‚ stretch‚ and walk around are crucial to prevent stiffness․ The NHS emphasizes the importance of avoiding prolonged pressure on the buttocks․ Consider using a cushion or adjusting seating to alleviate direct pressure․ Implementing these ergonomic adjustments minimizes strain and supports the benefits of prescribed exercises․
Activity Modification
Alongside NHS-recommended exercises found in PDF resources‚ modifying activities is crucial for piriformis syndrome recovery․ Temporarily reducing or avoiding activities that aggravate symptoms—like prolonged sitting‚ running‚ or certain hip movements—is essential․ Listen to your body and avoid pushing through pain‚ as this can worsen inflammation․
Gradually reintroduce activities as your pain subsides and strength improves․ Consider low-impact alternatives like swimming or cycling․ The NHS advises a phased return to activity‚ increasing intensity slowly․ Breaking down tasks into smaller segments with frequent breaks can also help․ Prioritizing rest and avoiding overexertion supports the healing process and prevents recurrence‚ complementing the exercise program․

Research and Recent Findings on Piriformis Syndrome Exercises
Studies analyze YouTube videos on piriformis syndrome exercises‚ assessing quality and reliability; NHS PDF resources offer structured‚ evidence-based exercise programs for optimal outcomes․
Research highlights the effectiveness of varied exercise approaches‚ including stretching‚ strengthening‚ and nerve flossing‚ aligning with NHS guidance for comprehensive treatment․
Evaluating online exercise guides is vital‚ ensuring they meet quality criteria and complement NHS recommendations for safe and effective piriformis syndrome management․
YouTube Video Quality Analysis
Recent research focused on evaluating the quality and reliability of YouTube videos demonstrating piriformis syndrome exercises․ The analysis aimed to identify criteria for selecting high-quality instructional content‚ a crucial aspect given the widespread use of online resources․ Findings revealed significant variability in the accuracy and safety of presented exercises․
Many videos lacked qualifications of the presenter‚ clear demonstration of proper form‚ or warnings regarding potential risks․ Conversely‚ higher-quality videos often featured qualified healthcare professionals and emphasized individualized exercise programs‚ potentially mirroring guidance found in NHS PDF resources․
The study underscores the importance of critical evaluation when utilizing YouTube for exercise instruction‚ recommending users prioritize videos from reputable sources and cross-reference information with trusted medical websites like the NHS‚ ensuring safe and effective self-management of piriformis syndrome․
Effectiveness of Different Exercise Approaches
Research suggests a multi-faceted approach to piriformis syndrome exercises yields the best results‚ combining stretching‚ strengthening‚ and nerve flossing techniques․ Stretching‚ like the figure-four stretch‚ aims to relieve muscle tension‚ while strengthening gluteal muscles provides support and stability․ Nerve flossing gently mobilizes the sciatic nerve‚ reducing irritation․
NHS guidance‚ often available in PDF format‚ typically advocates for a conservative management strategy prioritizing these exercise types․ The effectiveness varies individually; some respond well to stretching alone‚ while others require a comprehensive program․
Consistent adherence to a tailored exercise regimen is key‚ and consulting a physiotherapist ensures proper form and progression․ Combining these approaches‚ as outlined in reliable resources‚ maximizes the potential for pain reduction and improved function in individuals with piriformis syndrome․
